White Paper by Madelyn Robinson
Reviewed by Kritika Pathak, Khushboo Verma
Background
Intermittent fasting has gained a lot of attention in recent years for helping with weight loss, but what many people don’t know is that it’s not quite as simple as just eating less to lose a few pounds. Intermittent fasting is an umbrella term that describes a variety of eating patterns in which no or few calories are consumed for 12 to 48 hours on a recurring basis (Anton et al., 2017). These eating patterns include time restricted feeding (restriction of food intake to a 8-12 hour period of the day), alternate day fasting (alternation between little to no caloric intake one day and unrestricted caloric intake the next), and periodic fasting (fasting twice a week with unrestricted consumption of food during the other five days, also known as the 5:2 diet) (Barnosky et al., 2014; Longo & Panda, 2016; Bjarnadottir, 2018). Fasting is an integral practice in many different religious disciplines including Islam, Christianity, Judaism, and Hinduism, and it has been safely practiced for centuries (Lessan & Ali, 2019). In more recent years, however, fasting has become known for its health benefits as well.
Obesity and Metabolic Syndrome
Obesity is a complex and largely preventable disease, but about 30% of the world is obese or significantly overweight (Hruby & Hu, 2015). It is defined as a condition of abnormal or excessive fat accumulation in adipose tissue to the extent that health is impaired (Ofei, 2005). Obesity greatly increases the risk of chronic diseases such as depression, type 2 diabetes, cardiovascular disease, certain cancers, and mortality (Hu, 2008; Keipert et al., 2010). Obesity is also closely associated with metabolic syndrome, which affects 30-40% of people by age 65 (Han & Lean, 2016). Metabolic syndrome is a condition characterized by hypertension, central obesity, insulin resistance, elevated triglyceride and low-density lipoprotein (LDL) levels, and low high-density lipoprotein (HDL) levels, and it is strongly associated with an increased risk for developing diabetes and cardiovascular disease (Rochlani et al., 2017). It is widely accepted that fasting is effective at decreasing obesity and helping individuals lose weight; therefore, fasting can alleviate the effects of obesity as well, including those related to metabolic syndrome (Li et al., 2017; Harris et al., 2018; Zubrzycki et al., 2018; Templeton, 2019).
Metabolic Markers and Longevity
One of the main benefits of fasting is that it can favorably alter glucose and lipid metabolism and promote beneficial hormonal changes. Fasting shifts fuel utilization toward free fatty-acid mobilization, fatty-acid oxidation, and ketogenesis as glucose is conserved (Antoni et al., 2017). In fact, 12 to 24 hours of fasting typically results in a 20% decrease in serum glucose and depletion of the hepatic glycogen due to this switch in metabolic mode (Longo & Mattson, 2014). Metabolic and hormonal changes such as lower glucose, insulin, glycated hemoglobin, cholesterol, and blood pressure levels serve as metabolic markers, and all of these were seen in a study regarding the effects of fasting on humans (Walford et al., 2002). Since effects on human longevity are difficult to study, many studies regarding the effect of fasting on longevity in rats have been conducted and compared to shorter human studies (de Cabo et al., 2014; Antoni et al., 2017). Many of these rat studies not only concluded that fasting increases the longevity of rats, but they also concluded that many of the aforementioned metabolic markers seen in human fasting studies were also seen in these rats (Badreh et al., 2020; Carlson & Hoelzel, 1946; Mager et al., 2006).
Figure 2: Major responses of various organ systems to intermittent fasting (Anton et al., 2017).
Insulin sensitivity
One of the key factors in metabolic syndrome is insulin resistance, which is characterized by impaired glucose uptake in muscle and fat cells, reduced glycogen synthesis/storage in the liver, and failure to suppress hepatic glucose production (Barzilai & Ferrucci, 2012). Most likely caused by a post-receptor defect in target tissue insulin action, insulin resistance often develops with the aging process and is a major feature of type-2 diabetes (Evans & Goldfine, 2013; Fink et al., 1983). To counter the harmful effects of insulin resistance, the body needs to increase insulin sensitivity. Fasting has been shown to be an acceptable way to increase insulin sensitivity since body weight loss has been proven to improve insulin sensitivity and glucose tolerance (Sutton et al., 2018; Ryan, 2000; Barnosky et al., 2014; Cho et al., 2019). Increased insulin sensitivity reduces the effects of type-2 diabetes, which means that fasting can reduce the risk of diabetic complications such as heart attack, stroke, peripheral artery disease, nerve damage, retina damage, and kidney damage (IQWiG, 2008).
Reducing Cardiovascular Disease Risk Factors
Studies have suggested that alternate day fasting can reduce risk factors associated with cardiovascular disease (Tinsley & La Bounty, 2015). Many human clinical trials have resulted in the reduction of total cholesterol, LDL, and triglycerides, although not in every single case (Johnson et al., 2007; Varady et al., 2009; Varady et al., 2011; Klemel et al., 2013). Total cholesterol consists of LDL, HDL, and very low-density lipoprotein (VLDL), and maintaining cholesterol and triglyceride levels within healthy limits is critical for decreasing the risk of heart disease (Elshourbagy et al., 2013). While HDL is beneficial to the body, LDL drives the development of atherosclerosis, which can contribute to heart attacks and strokes (Ravnskov, 2002). Elevated triglyceride levels also contribute to cardiovascular disease by increasing inflammation and artherosclerotic plaque formation, and triglycerides have also been proven to be risk factors for cognitive decline as well (Singh & Singh, 2016; Parthasarathy et al., 2017). Therefore, fasting can very possibly reduce the negative cardiac and cognitive decline that is associated with aging by reducing LDL cholesterol and triglyceride levels.
Therapy in Neurodegeneration
Aging is associated with neurodegenerative disorders such as Parkinson’s disease, Alzheimer’s disease, and Huntington’s disease, and these disorders are linked to impaired glucose metabolism, neuron bioenergetics, insulin signaling, and neurotrophic signaling (Phillips, 2019; Mattson et al., 2017). Fasting has been shown to slow neurodegeneration in animal models of Parkinson’s disease, Alzheimer’s disease, and Huntington’s disease by protecting neurons from mitochondrial toxins and kainic acid (Duan & Mattson, 1999; Anson et al., 2003). These rodents were seen to have improved cognition and slowed cognitive decline (Fontan-Lozano et al., 2007; Li et al., 2013). Fasting’s effects on neurodegeneration in humans are still largely untested, but many researchers hopefully await future research into the subject due to the strength of animal evidence (Phillips, 2019).
Anti-Cancer Effects
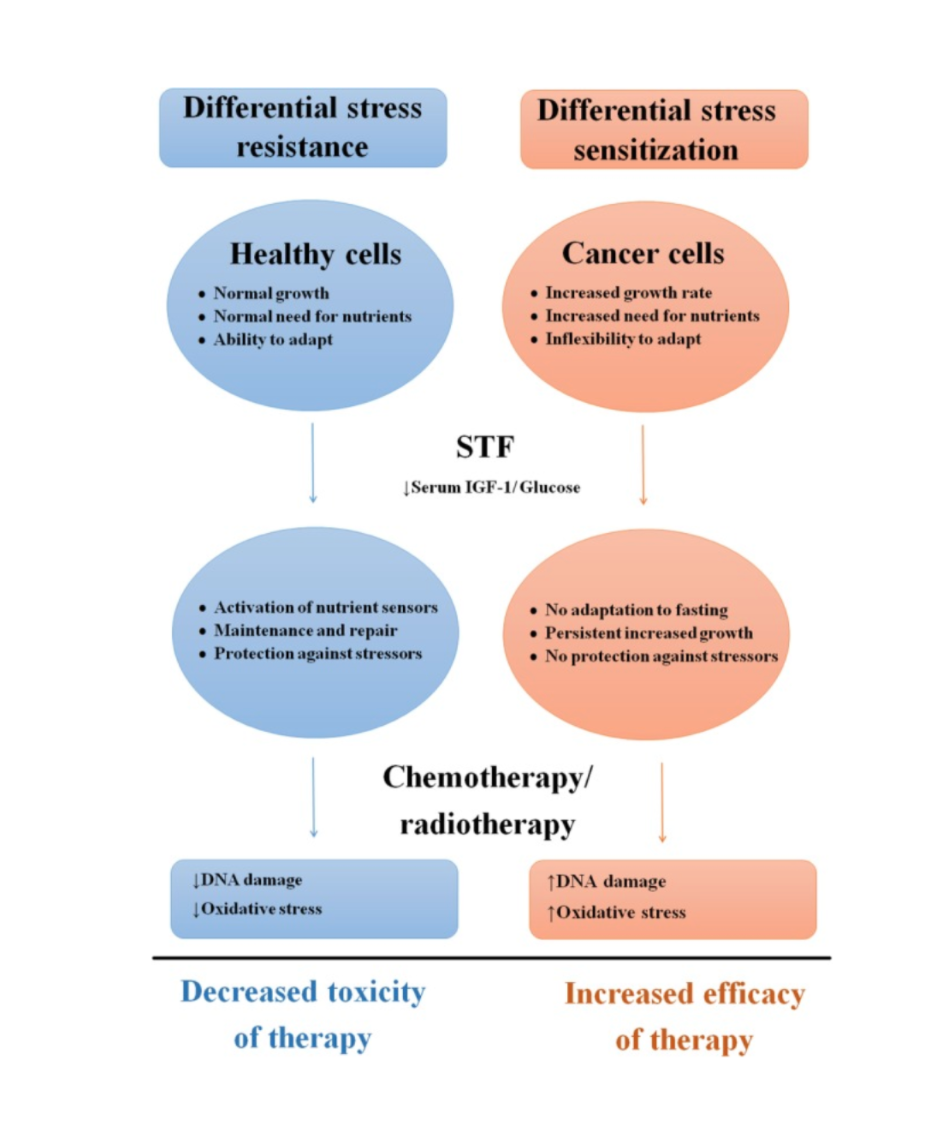
Furthermore, many clinical studies have concluded that fasting and caloric restriction reduces cancer incidence and inhibits tumor progression in rodents (Dirx et al., 2003; De Lorenzo et al., 2011; Lv et al., 2014; Mai et al., 2003), strongly reduces cancer incidence and mortality in primates (Colman et al., 2009), and reduces metabolic and hormonal factors linked to cancer risks in humans (Renehan et al., 2004; Ravussin et al., 2015). Of course, fasting alone is not an effective treatment or sole preventative measure against cancer, but it can be a useful supplement to mainstream treatment especially since fasting has also been shown to protect from chemotherapy’s toxic effects in numerous rodent studies (de Groot et al., 2019; Brandhorst et al., 2013; Tinkum et al., 2015; Huisman et al., 2015). This is largely because fasting reinforces the stress resistance of healthy cells while imposing extra stress on tumor cells; the stress on tumor cells results from the switch to oxidative metabolic phenotype that fasting encourages instead of the natural glycolytic metabolism that helps tumors resist radiation (Klement, 2015; Di Biase et al., 2017; de Groot et al., 2019).
Figure 3: Effects of short-term fasting on healthy and cancerous cells (de Groot et al., 2019).
Risks and Safety Concerns
However, intermittent fasting has also been shown to have a few risks and safety concerns. Firstly, it can lead to fatigue, dizziness, and difficulty concentrating in the long run, even though it might increase alertness short term, if the body is simply not getting the energy it needs (Meszaros, 2020). Furthermore, intermittent fasting can increase cortisol levels, the body’s stress hormone, which is often associated with increased stress, increased fat storage, and decreased insulin sensitivity, especially in overweight individuals (Adam et al., 2010; van der Valk et al., 2018). When taken to the extreme, fasting can even lead to ketoacidosis (Blanco et al., 2019). Fasting induces ketosis after about 12 hours, and this is considered harmless because few ketone bodies are generated (Masood, 2020). However, in ketoacidosis, the liver generates enough ketone bodies to lower blood pH and is life threatening; it generally takes about 3-14 days of complete fasting to reach the maximum severity of ketoacidosis (Nickson, 2019). Finally, intermittent fasting can lead to disordered eating behaviors such as orthorexia, which is the unhealthy obsession with eating healthy, or anorexia, which is compulsive fasting to lose weight (Petre, 2020). Despite these potential adverse effects, however, the majority of adverse effects of fasting are generally mild to moderate (Finnell et al., 2018).
Conclusion
Fasting, a practice in which little to no calories are consumed during a defined period of time, has been around for centuries, and it is no surprise that it has health benefits in addition to cultural importance. These health benefits include decreasing the effects of obesity and metabolic syndrome, producing beneficial metabolic and hormonal changes, increasing insulin sensitivity (and thus alleviating the effects of type-2 diabetes), reducing risk factors for cardiovascular disease, potentially slowing cognitive decline, and decreasing the toxicity while increasing the efficacy of cancer therapies. While largely considered safe, intermittent fasting does have some mild to moderate risks, so it is recommended to consult a health professional prior to starting to fast.
References
Adam, T. C., Hasson, R. E., Ventura, E. E., Toledo-Corral, C., Le, K.-A., Mahurkar, S., Lane, C. J., Weigensberg, M. J., & Goran, M. I. (2010). Cortisol Is Negatively Associated with Insulin Sensitivity in Overweight Latino Youth. The Journal of Clinical Endocrinology & Metabolism, 95(10), 4729–4735. https://doi.org/10.1210/jc.2010-0322
Anson, R. M., Guo, Z., de Cabo, R., Iyun, T., Rios, M., Hagepanos, A., Ingram, D. K., Lane, M. A., & Mattson, M. P. (2003). Intermittent fasting dissociates beneficial effects of dietary restriction on glucose metabolism and neuronal resistance to injury from calorie intake. Proceedings of the National Academy of Sciences, 100(10), 6216–6220. https://doi.org/10.1073/pnas.1035720100
Anton, S. D., Moehl, K., Donahoo, W. T., Marosi, K., Lee, S. A., Mainous, A. G., Leeuwenburgh, C., & Mattson, M. P. (2017). Flipping the Metabolic Switch: Understanding and Applying the Health Benefits of Fasting. Obesity, 26(2), 254–268. https://doi.org/10.1002/oby.22065
Antoni, R., Johnston, K. L., Collins, A. L., & Robertson, M. D. (2017). Effects of intermittent fasting on glucose and lipid metabolism. Proceedings of the Nutrition Society, 76(3), 361–368. https://doi.org/10.1017/s0029665116002986
Badreh, F., Joukar, S., Badavi, M., Rashno, M., & Dehesh, T. (2020). The Effects of Age and Fasting Models on Blood Pressure, Insulin/Glucose Profile, and Expression of Longevity Proteins in Male Rats. Rejuvenation Research, 23(3), 224–236. https://doi.org/10.1089/rej.2019.2205
Barnosky, A. R., Hoddy, K. K., Unterman, T. G., & Varady, K. A. (2014). Intermittent fasting vs daily calorie restriction for type 2 diabetes prevention: a review of human findings. Translational Research, 164(4), 302–311. https://doi.org/10.1016/j.trsl.2014.05.013
Barzilai, N., & Ferrucci, L. (2012). Insulin Resistance and Aging: A Cause or a Protective Response? The Journals of Gerontology Series A: Biological Sciences and Medical Sciences, 67(12), 1329–1331. https://doi.org/10.1093/gerona/gls145
Bjarnadottir, A. (2018, May 31). The Beginner’s Guide to the 5:2 Diet. Healthline. https://www.healthline.com/nutrition/the-5-2-diet-guide#section2
Blanco, J. C., Khatri, A., Kifayat, A., Cho, R., & Aronow, W. S. (2019). Starvation Ketoacidosis due to the Ketogenic Diet and Prolonged Fasting – A Possibly Dangerous Diet Trend. American Journal of Case Reports, 20, 1728–1731. https://doi.org/10.12659/ajcr.917226
Brandhorst, S., Wei, M., Hwang, S., Morgan, T. E., & Longo, V. D. (2013). Short-term calorie and protein restriction provide partial protection from chemotoxicity but do not delay glioma progression. Experimental Gerontology, 48(10), 1120–1128. https://doi.org/10.1016/j.exger.2013.02.016
Carlson, A. J., & Hoelzel, F. (1946). Apparent Prolongation of the Life Span of Rats by Intermittent Fasting. The Journal of Nutrition, 31(3), 363–375. https://doi.org/10.1093/jn/31.3.363
Cho, Y., Hong, N., Kim, K., Cho, S., Lee, M., Lee, Y., Lee, Y., Kang, E., Cha, B.-S., & Lee, B.-W. (2019). The Effectiveness of Intermittent Fasting to Reduce Body Mass Index and Glucose Metabolism: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 8(10), 1645. https://doi.org/10.3390/jcm8101645
Colman, R. J., Anderson, R. M., Johnson, S. C., Kastman, E. K., Kosmatka, K. J., Beasley, T. M., Allison, D. B., Cruzen, C., Simmons, H. A., Kemnitz, J. W., & Weindruch, R. (2009). Caloric Restriction Delays Disease Onset and Mortality in Rhesus Monkeys. Science, 325(5937), 201–204. https://doi.org/10.1126/science.1173635
de Cabo, R., Carmona-Gutierrez, D., Bernier, M., Hall, M. N., & Madeo, F. (2014). The Search for Antiaging Interventions: From Elixirs to Fasting Regimens. Cell, 157(7), 1515–1526. https://doi.org/10.1016/j.cell.2014.05.031
de Groot, S., Pijl, H., van der Hoeven, J. J. M., & Kroep, J. R. (2019). Effects of short-term fasting on cancer treatment. Journal of Experimental & Clinical Cancer Research, 38(1), 209. https://doi.org/10.1186/s13046-019-1189-9
De Lorenzo, M. S., Baljinnyam, E., Vatner, D. E., Abarzua, P., Vatner, S. F., & Rabson, A. B. (2011). Caloric restriction reduces growth of mammary tumors and metastases. Carcinogenesis, 32(9), 1381–1387. https://doi.org/10.1093/carcin/bgr107
Di Biase, S., Shim, H. S., Kim, K. H., Vinciguerra, M., Rappa, F., Wei, M., Brandhorst, S., Cappello, F., Mirzaei, H., Lee, C., & Longo, V. D. (2017). Fasting regulates EGR1 and protects from glucose- and dexamethasone-dependent sensitization to chemotherapy. PLOS Biology, 15(3), e2001951. https://doi.org/10.1371/journal.pbio.2001951
Di Francesco, A., Di Germanio, C., Bernier, M., & de Cabo, R. (2018). A time to fast. Science, 362(6416), 770–775. https://doi.org/10.1126/science.aau2095
Dirx, M. J. M., Zeegers, M. P. A., Dagnelie, P. C., van den Bogaard, T., & van den Brandt, P. A. (2003). Energy restriction and the risk of spontaneous mammary tumors in mice: A meta-analysis. International Journal of Cancer, 106(5), 766–770. https://doi.org/10.1002/ijc.11277
Duan, W., & Mattson, M. P. (1999). Dietary restriction and 2-deoxyglucose administration improve behavioral outcome and reduce degeneration of dopaminergic neurons in models of Parkinson’s disease. Journal of Neuroscience Research, 57(2), 195–206. https://doi.org/10.1002/(SICI)1097-4547(19990715)57:2<195::AID-JNR5>3.0.CO;2-P
Elshourbagy, N. A., Meyers, H. V., & Abdel-Meguid, S. S. (2013). Cholesterol: The Good, the Bad, and the Ugly - Therapeutic Targets for the Treatment of Dyslipidemia. Medical Principles and Practice, 23(2), 99–111. https://doi.org/10.1159/000356856
Evans, J. L., & Goldfine, I. D. (2013). Aging and Insulin Resistance: Just Say iNOS. Diabetes, 62(2), 346–348. https://doi.org/10.2337/db12-1239
Fink, R. I., Kolterman, O. G., Griffin, J., & Olefsky, J. M. (1983). Mechanisms of Insulin Resistance in Aging. Journal of Clinical Investigation, 71(6), 1523–1535. https://doi.org/10.1172/jci110908
Finnell, J. S., Saul, B. C., Goldhamer, A. C., & Myers, T. R. (2018). Is fasting safe? A chart review of adverse events during medically supervised, water-only fasting. BMC Complementary and Alternative Medicine, 18(1), . https://doi.org/10.1186/s12906-018-2136-6
Fontan-Lozano, A., Saez-Cassanelli, J. L., Inda, M. C., de los Santos-Arteaga, M., Sierra-Dominguez, S. A., Lopez-Lluch, G., Delgado-Garcia, J. M., & Carrion, A. M. (2007). Caloric Restriction Increases Learning Consolidation and Facilitates Synaptic Plasticity through Mechanisms Dependent on NR2B Subunits of the NMDA Receptor. Journal of Neuroscience, 27(38), 10185–10195. https://doi.org/10.1523/jneurosci.2757-07.2007
Han, T. S., & Lean, M. E. J. (2016). A clinical perspective of obesity, metabolic syndrome and cardiovascular disease. JRSM Cardiovascular Disease, 5, 204800401663337. https://doi.org/10.1177/2048004016633371
Harris, L., Hamilton, S., Azevedo, L. B., Olajide, J., De Brún, C., Waller, G., Whittaker, V., Sharp, T., Lean, M., Hankey, C., & Ells, L. (2018). Intermittent fasting interventions for treatment of overweight and obesity in adults. JBI Database of Systematic Reviews and Implementation Reports, 16(2), 507–547. https://doi.org/10.11124/jbisrir-2016-003248
Hruby, A., & Hu, F. B. (2015). The Epidemiology of Obesity: A Big Picture. PharmacoEconomics, 33(7), 673–689. https://doi.org/10.1007/s40273-014-0243-x
Hu, F. (2008). Obesity Epidemiology (1st ed.). Oxford University Press.
Institute for Quality and Efficiency in Health Care (IQWiG). (2008). Type 2 diabetes: Overview. Informed Health.
Johnson, J. B., Summer, W., Cutler, R. G., Martin, B., Hyun, D.-H., Dixit, V. D., Pearson, M., Nassar, M., Tellejohan, R., Maudsley, S., Carlson, O., John, S., Laub, D. R., & Mattson, M. P. (2007). Alternate day calorie restriction improves clinical findings and reduces markers of oxidative stress and inflammation in overweight adults with moderate asthma. Free Radical Biology and Medicine, 42(5), 665–674. https://doi.org/10.1016/j.freeradbiomed.2006.12.005
Keipert, S., Voigt, A., & Klaus, S. (2010). Dietary effects on body composition, glucose metabolism, and longevity are modulated by skeletal muscle mitochondrial uncoupling in mice. Aging Cell, 10(1), 122–136. https://doi.org/10.1111/j.1474-9726.2010.00648.x
Klement, R. J. (2017). Fasting, Fats, and Physics: Combining Ketogenic and Radiation Therapy against Cancer. Complementary Medicine Research, 25(2), 102–113. https://doi.org/10.1159/000484045
Klempel, M. C., Kroeger, C. M., & Varady, K. A. (2013). Alternate day fasting (ADF) with a high-fat diet produces similar weight loss and cardio-protection as ADF with a low-fat diet. Metabolism, 62(1), 137–143. https://doi.org/10.1016/j.metabol.2012.07.002
Lessan, N., & Ali, T. (2019). Energy Metabolism and Intermittent Fasting: The Ramadan Perspective. Nutrients, 11(5), 1192. https://doi.org/10.3390/nu11051192
Li, G., Xie, C., Lu, S., Nichols, R. G., Tian, Y., Li, L., Patel, D., Ma, Y., Brocker, C. N., Yan, T., Krausz, K. W., Xiang, R., Gavrilova, O., Patterson, A. D., & Gonzalez, F. J. (2017). Intermittent Fasting Promotes White Adipose Browning and Decreases Obesity by Shaping the Gut Microbiota. Cell Metabolism, 26(4), 672–685. https://doi.org/10.1016/j.cmet.2017.08.019
Longo, V. D., & Mattson, M. P. (2014). Fasting: Molecular Mechanisms and Clinical Applications. Cell Metabolism, 19(2), 181–192. https://doi.org/10.1016/j.cmet.2013.12.008
Longo, V. D., & Panda, S. (2016). Fasting, Circadian Rhythms, and Time-Restricted Feeding in Healthy Lifespan. Cell Metabolism, 23(6), 1048–1059. https://doi.org/10.1016/j.cmet.2016.06.001
Mager, D. E., Wan, R., Brown, M., Cheng, A., Wareski, P., Abernethy, D. R., & Mattson, M. P. (2006). Caloric restriction and intermittent fasting alter spectral measures of heart rate and blood pressure variability in rats. The FASEB Journal, 20(6), 631–637. https://doi.org/10.1096/fj.05-5263com
Mai, V., Colbert, L. H., Berrigan, D., Perkins, S. N., Pfeiffer, R., Lavigne, J. A., Lanza, E., Haines, D. C., Schatzkin, A., & Hursting, S. D. (2003). Cancer Research (8th ed., Vol. 63). American Association for Cancer Research.
Masood, W. (2020, June 22). Ketogenic Diet - StatPearls - NCBI Bookshelf. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK499830/
Mattson, M. P., Longo, V. D., & Harvie, M. (2017). Impact of intermittent fasting on health and disease processes. Ageing Research Reviews, 39, 46–58. https://doi.org/10.1016/j.arr.2016.10.005
Meszaros, L. (2020, January 8). The Dangers of Intermittent Fasting. MDLinx. https://www.mdlinx.com/article/the-dangers-of-intermittent-fasting/6CZfO5sYFDWi4wK2OPRiEd
Nickson, C. (2019, March 20). Ketoacidosis. Life in the Fastlane. https://litfl.com/ketoacidosis/#:~:text=1.-,STARVATION%20KETOSIS,starvation%20to%20reach%20maximal%20severity
Ofei F. (2005). Obesity - a preventable disease. Ghana medical journal, 39(3), 98–101.
Parthasarathy, V., Frazier, D. T., Bettcher, B. M., Jastrzab, L., Chao, L., Reed, B., Mungas, D., Weiner, M., DeCarli, C., Chui, H., & Kramer, J. H. (2017). Triglycerides are negatively correlated with cognitive function in nondemented aging adults. Neuropsychology, 31(6), 682–688. https://doi.org/10.1037/neu0000335
Petre, A. (2020, April 2). Orthorexia: When Healthy Eating Becomes a Disorder. Healthline. https://www.healthline.com/nutrition/orthorexia-nervosa-101
Phillips. (2019). Fasting as a Therapy in Neurological Disease. Nutrients, 11(10), 2501. https://doi.org/10.3390/nu11102501
Ravnskov, U. (2002). Is atherosclerosis caused by high cholesterol? QJM, 95(6), 397–403. https://doi.org/10.1093/qjmed/95.6.397
Ravussin, E., Redman, L. M., Rochon, J., Das, S. K., Fontana, L., Kraus, W. E., Romashkan, S., Williamson, D. A., Meydani, S. N., Villareal, D. T., Smith, S. R., Stein, R. I., Scott, T. M., Stewart, T. M., Saltzman, E., Klein, S., Bhapkar, M., Martin, C. K., Gilhooly, C. H., … Roberts, S. B. (2015). A 2-Year Randomized Controlled Trial of Human Caloric Restriction: Feasibility and Effects on Predictors of Health Span and Longevity. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences, 70(9), 1097–1104. https://doi.org/10.1093/gerona/glv057
Renehan, A. G., Zwahlen, M., Minder, C., O’Dwyer, S. T., Shalet, S. M., & Egger, M. (2004). Insulin-like growth factor (IGF)-I, IGF binding protein-3, and cancer risk: systematic review and meta-regression analysis. The Lancet, 363(9418), 1346–1353. https://doi.org/10.1016/s0140-6736(04)16044-3
Rochlani, Y., Pothineni, N. V., Kovelamudi, S., & Mehta, J. L. (2017). Metabolic syndrome: pathophysiology, management, and modulation by natural compounds. Therapeutic Advances in Cardiovascular Disease, 11(8), 215–225. https://doi.org/10.1177/1753944717711379
Ryan, A. S. (2000). Insulin Resistance with Aging. Sports Medicine, 30(5), 327–346. https://doi.org/10.2165/00007256-200030050-00002
Singh, A., & Singh, R. (2016). Triglyceride and cardiovascular risk: A critical appraisal. Indian Journal of Endocrinology and Metabolism, 20(4), 418. https://doi.org/10.4103/2230-8210.183460
Sutton, E. F., Beyl, R., Early, K. S., Cefalu, W. T., Ravussin, E., & Peterson, C. M. (2018). Early Time-Restricted Feeding Improves Insulin Sensitivity, Blood Pressure, and Oxidative Stress Even without Weight Loss in Men with Prediabetes. Cell Metabolism, 27(6), 1212–1221. https://doi.org/10.1016/j.cmet.2018.04.010
Tinkum, K. L., Stemler, K. M., White, L. S., Loza, A. J., Jeter-Jones, S., Michalski, B. M., Kuzmicki, C., Pless, R., Stappenbeck, T. S., Piwnica-Worms, D., & Piwnica-Worms, H. (2015). Fasting protects mice from lethal DNA damage by promoting small intestinal epithelial stem cell survival. Proceedings of the National Academy of Sciences, 112(51), 7148–7154. https://doi.org/10.1073/pnas.1509249112
Templeton, L. (2019, December 28). Intermittent fasting can help ease metabolic syndrome. Medical News Today. https://www.medicalnewstoday.com/articles/327247
Tinsley, G. M., & La Bounty, P. M. (2015). Effects of intermittent fasting on body composition and clinical health markers in humans. Nutrition Reviews, 73(10), 661–674. https://doi.org/10.1093/nutrit/nuv041
van der Valk, E. S., Savas, M., & van Rossum, E. F. C. (2018). Stress and Obesity: Are There More Susceptible Individuals? Current Obesity Reports, 7(2), 193–203. https://doi.org/10.1007/s13679-018-0306-y
Varady, K. A., Bhutani, S., Church, E. C., & Klempel, M. C. (2009). Short-term modified alternate-day fasting: a novel dietary strategy for weight loss and cardioprotection in obese adults. The American Journal of Clinical Nutrition, 90(5), 1138–1143. https://doi.org/10.3945/ajcn.2009.28380
Varady, K. A., Bhutani, S., Klempel, M. C., & Kroeger, C. M. (2011). Comparison of effects of diet versus exercise weight loss regimens on LDL and HDL particle size in obese adults. Lipids in Health and Disease, 10(1), 119. https://doi.org/10.1186/1476-511x-10-119
Walford, R. L., Mock, D., Verdery, R., & MacCallum, T. (2002). Calorie Restriction in Biosphere 2: Alterations in Physiologic, Hematologic, Hormonal, and Biochemical Parameters in Humans Restricted for a 2-Year Period. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences, 57(6), 211–224. https://doi.org/10.1093/gerona/57.6.b211
Zubrzycki, A., Cierpka-Kmiec, K., Kmiec, Z., & Wronska, A. (2018). The role of low-calorie diets and intermittent fasting in the treatment of obesity and type-2 diabetes. Journal of Physiology and Pharmacology, 69(5), 663–683. https://doi.org/10.26402/jpp.2018.5.02